5th ISTANBUL SYMPOSIUM: BIOENGINEERING APPROACHES ON PEDIATRIC CARDIOVASCULAR MEDICINE – Koç University, Sevgi Gönül Auditorium – 21 December 2012
Scientific Co-Chairs are Kerem Pekkan, PhD & Akif Ündar, PhD
Invitation to Attend
The 5th Istanbul Symposium is intended for medical and engineering students, nurses,
scientists, pediatric heart surgeons, engineers, cardiologists, intensivists, neonatologists,
anesthesiologists, neurologists, pediatric perfusionists, respiratory therapists, residents
and fellows. All are invited and encouraged to attend.
Invited Faculty
Mehmet A. Ağırbaşlı, MD Dept. of Cardiology, Marmara University, Istanbul, Türkiye
Atıf Akçevin, MD Dept. of Cardiovascular Surgery, Medipol University, Istanbul, Türkiye
Tijen Alkan-Bozkaya, MD Dept. of Cardiovascular Surgery, Medipol University, Istanbul, Türkiye
Ihsan Bakır, MD Istanbul Mehmet Akif Ersoy Thoracic and Cardiovascular
Surgery Training and Research Hospital, Istanbul, Türkiye
Hakan Ceyran, MD Istanbul Koşuyolu Heart Hospital, Cardiovascular Surgery,
Istanbul, Türkiye
Sertaç Haydın, MD Istanbul Mehmet Akif Ersoy Thoracic and Cardiovascular
Surgery Training and Research Hospital, Istanbul, Türkiye
Ender Ödemiş, MD Istanbul Mehmet Akif Ersoy Thoracic and Cardiovascular
Surgery Training and Research Hospital, Istanbul, Türkiye
Kerem Pekkan, PhD Şevket Ruacan, MD, Dept. Of Mechanical Engineering, Koc University, Istanbul,
Türkiye
Dean, College of Medicine, Koç University, Istanbul, Türkiye
Ayda Türköz, MD Başkent University, Department of Anethesiology, Istanbul,
Türkiye
Rıza Türköz, MD Başkent University, Department of Cardiovascular Surgery,
Istanbul, Türkiye
Akif Ündar, PhD Penn State Hershey Pediatric Cardiovascular Research
Center, Penn State Hershey College of Medicine, Penn State
Hershey Children’s Hospital, Hershey, PA, USA
Songül Yaşar Yıldız, PhD Candidate Dept. of Bioengineeering, Marmara University,
Istanbul, Türkiye)
TBA (Koç University, School of Nursing, Istanbul, Türkiye
3
SCIENTIFIC PROGRAM
9:00 ? 9:20 am Welcome ? Kerem Pekkan, PhD& Şevket Ruacan, MD, Dean, College of Medicine, Koç University,
Istanbul, Türkiye
9:20 ? 10:00 am ABC’s of Pediatric Cardiovascular Research for Medical and
Engineering Students
Akif Ündar, PhD ? Penn State Hershey Pediatric Cardiovascular
Research Center, Penn State Hershey College of Medicine, Penn
State Hershey Children’s Hospital, Hershey, PA, USA
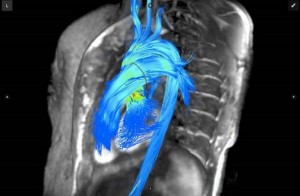
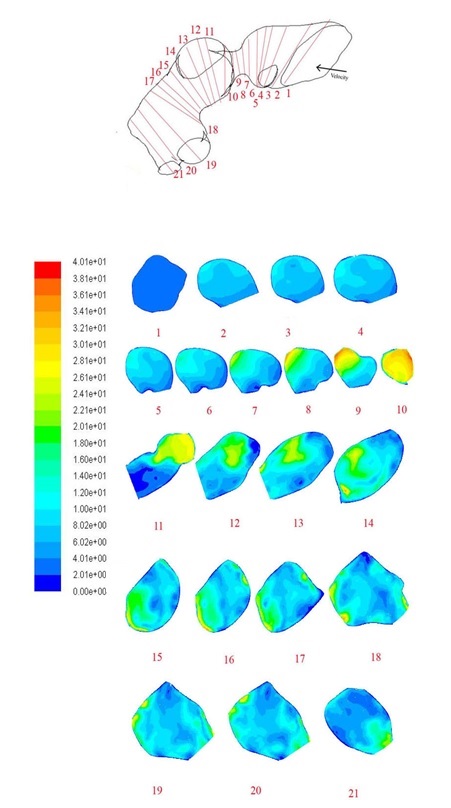
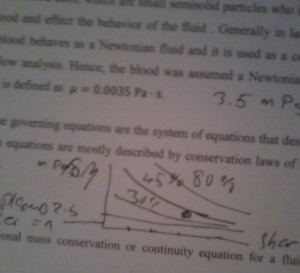
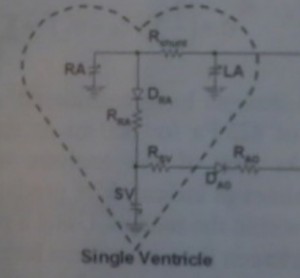
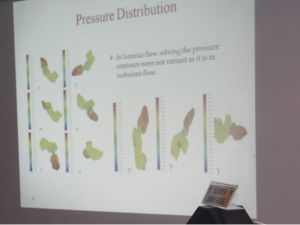
10:00 ? 11:00 am Key Note Lecture – Applications of Computational Fluid Dynamics to
solve pediatric cardiovascular problems
Kerem Pekkan, PhD, (Dept. Of Mechanical Engineering, Koc
University, Istanbul, Türkiye)
Introduction: Akif Ündar, PhD
11:00 ? 11: 15 am Break
11:15 am ? Noon CASE STUDY: Novel fenestration designs for controlled venous flow
shunting in failing Fontans with systemic hypertension
Cardiac Surgeon: Definition of the problem – Rıza Türköz, MD
(Başkent University, Department of Cardiovascular Surgery, Istanbul,
Türkiye)
Scientist: Suggested Solution – Kerem Pekkan, PhD
12:00 ? 13:30 pm Lunch
13:30 ? 14:00 pm What are the "real" problems for pediatric cardiac patients in
Türkiye? Why multi-disciplinary approach is necessity, not an option?
Atıf Akçevin, MD (Dept. of Cardiovascular Surgery, Medipol
University, Istanbul)
14:00 ? 15:30 pm PANEL: Importance of Multidisciplinary Team Approach to Improve
the Outcomes During and After Neonatal and Pediatric
Cardiopulmonary Bypass Procedures in Türkiye
Moderators: Atıf Akçevin, MD and Ihsan Bakır, MD
4
Pediatric Cardiologists’ Perspective – Ender Ödemiş, MD (Istanbul
Mehmet Akif Ersoy Thoracic and Cardiovascular Surgery Training and
Research Hospital, Istanbul, Türkiye) (20 min)
Pediatric Cardiac Surgeons’ Perspective – Hakan Ceyran, MD (Istanbul
Koşuyolu Heart Hospital, Cardiovascular Surgery, Istanbul, Türkiye)
(20 min)
Pediatric Anesthesiologists’ Perspective – Ayda Türköz, MD (Başkent University, Department of Anethesiology, Istanbul, Türkiye)
(20 min)
Pediatric Nurses’ Perspective – TBA (Koç University, School of Nursing, Istanbul, Türkiye (20 min)
15:30 ? 16:00pm Break
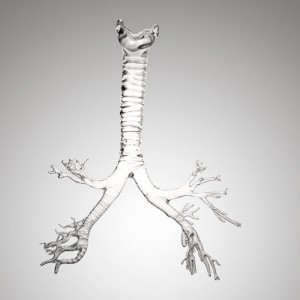
16:00 ? 18:00pm PANEL: Pediatric ECLS Systems & Novel Techniques and Methods to
Minimize the Injury during neonatal/Pediatric Cardiopulmonary
Bypass Procedures
Moderators: Hakan Ceyran, MD and Rıza Türköz, MD
Pediatric Extracorporeal Life Support Systems in Türkiye ? 2012
Update –
Sertaç Haydın, MD (Istanbul Mehmet Akif Ersoy Thoracic and
Cardiovascular Surgery Training and Research Hospital, Istanbul,
Türkiye)
Monitoring Biomarkers After Pediatric Cardiac Surgery: A New
Paradigm in the Horizon, Mehmet A. Ağırbaşlı, MD (Dept. of
Cardiology, Marmara University, Istanbul, Türkiye)
Extremophiles for cardiovascular research – Songül Yaşar Yıldız, PhD
Candidate (Dept. of Bioengineeering, Marmara University, Istanbul,
Türkiye)
Impact of Pulsatile Perfusion on Clinical Outcomes of Neonates and
infants with Complex Pathologies undergoing Cardiopulmonary
Bypass Procedures ?
Tijen Alkan-Bozkaya, MD (Dept. of Cardiovascular Surgery, Medipol
University, Istanbul)
5
Importance of Neonatal/Pediatric oxygenators with or without
Arterial Filters for capturing microemboli during CPB procedures –
Akif Ündar, PhD
18:00pm Closing Remarks – Kerem Pekkan, PhD
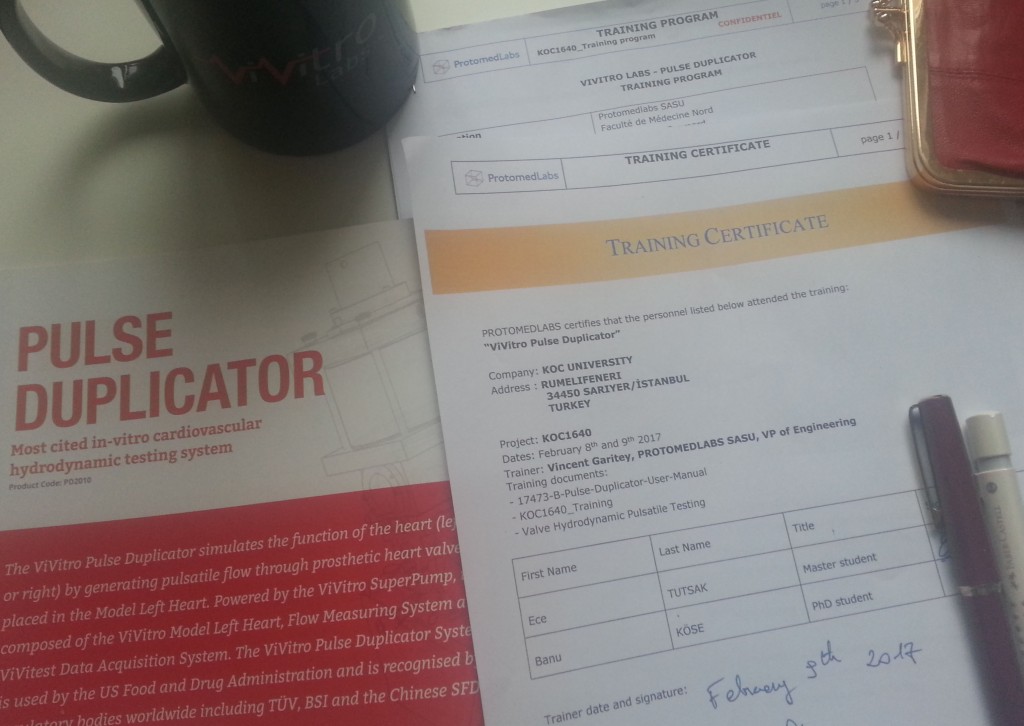
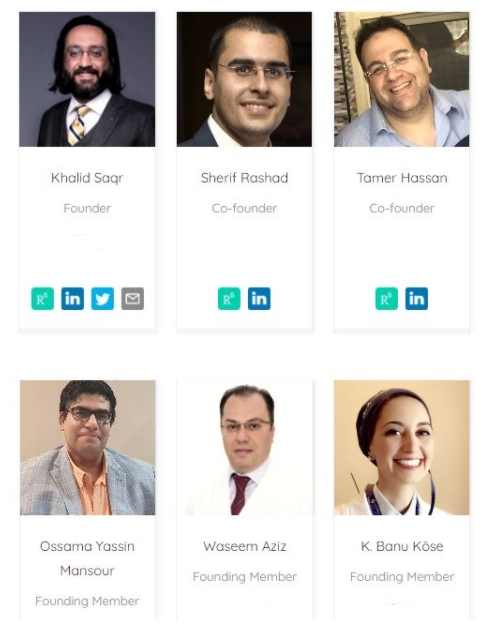
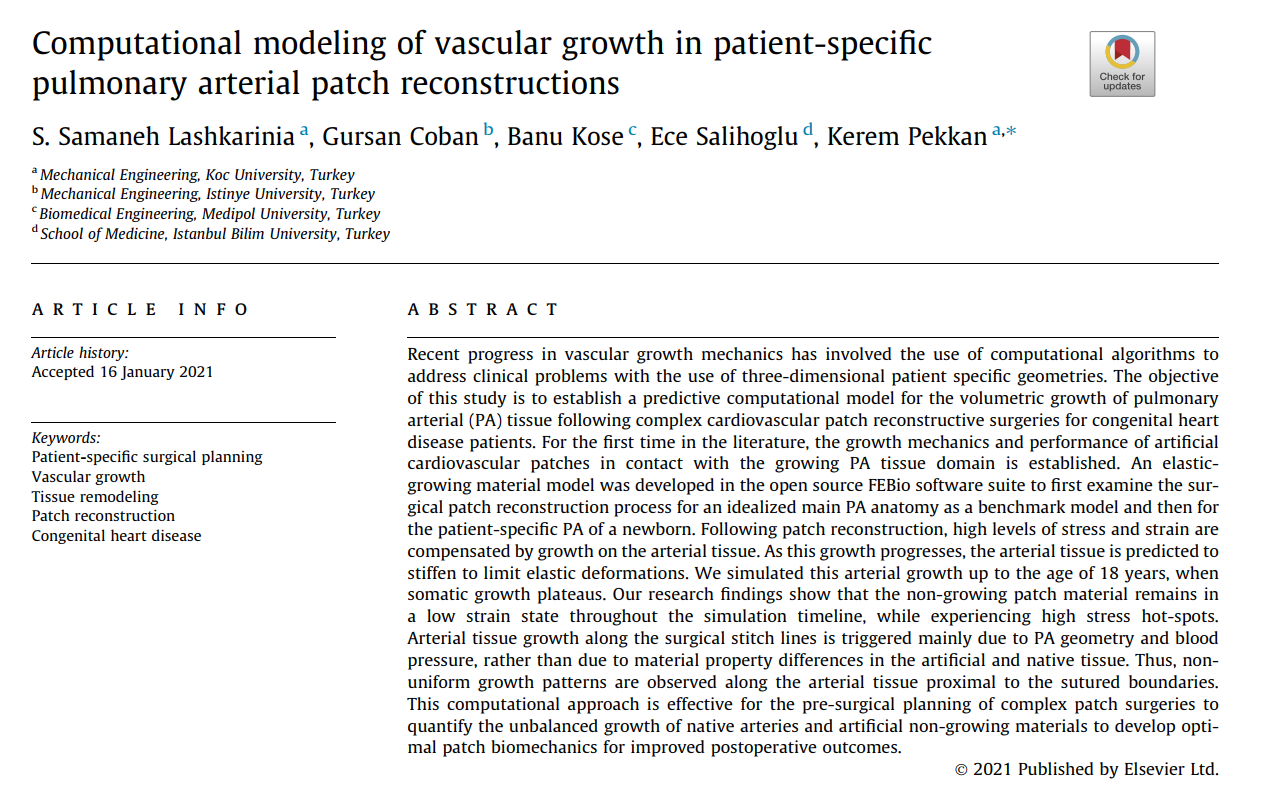
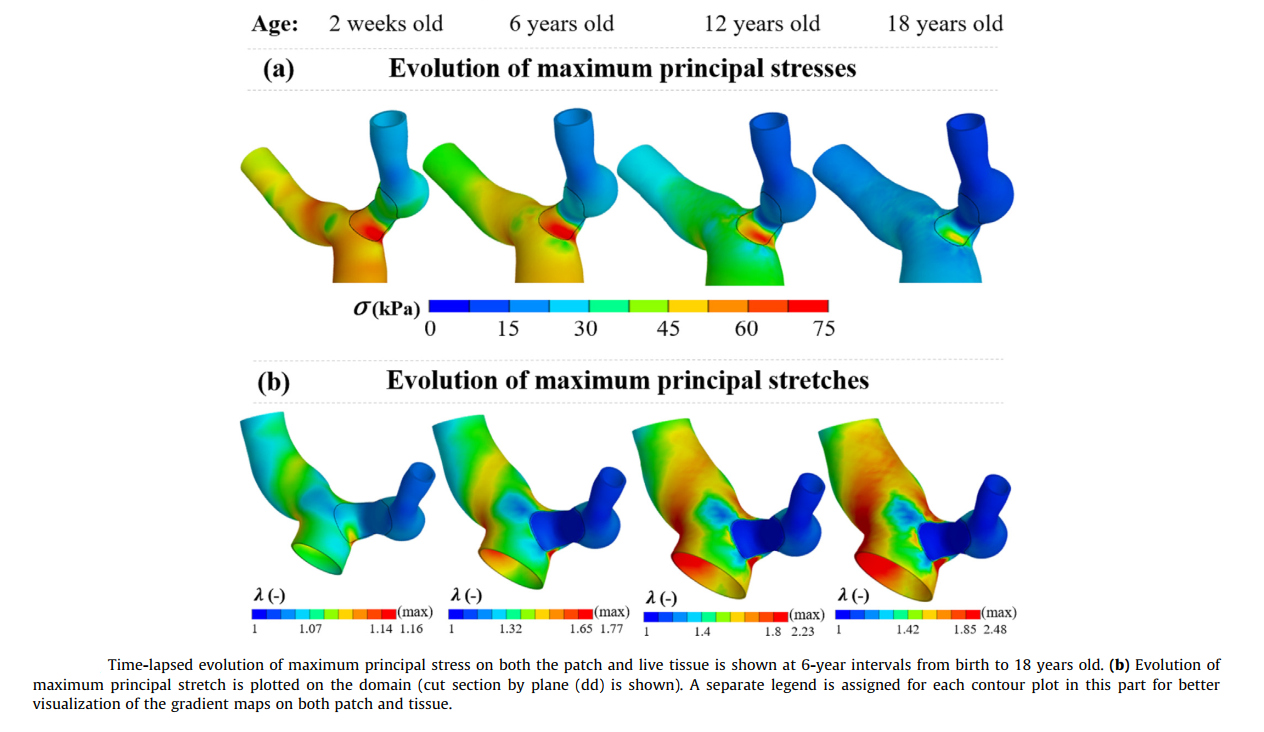
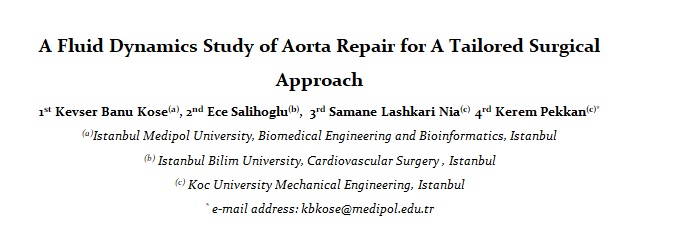
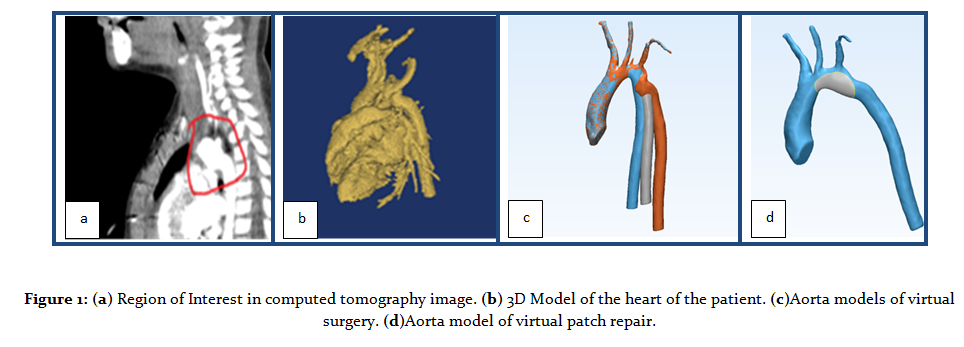
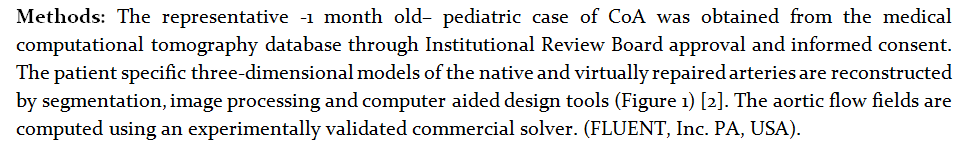
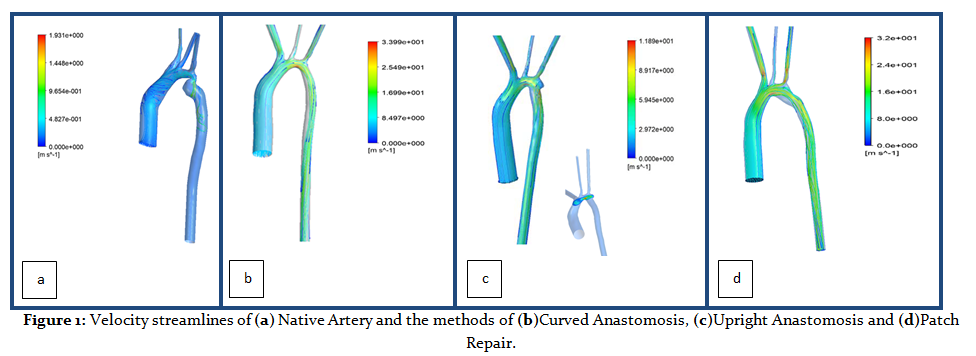
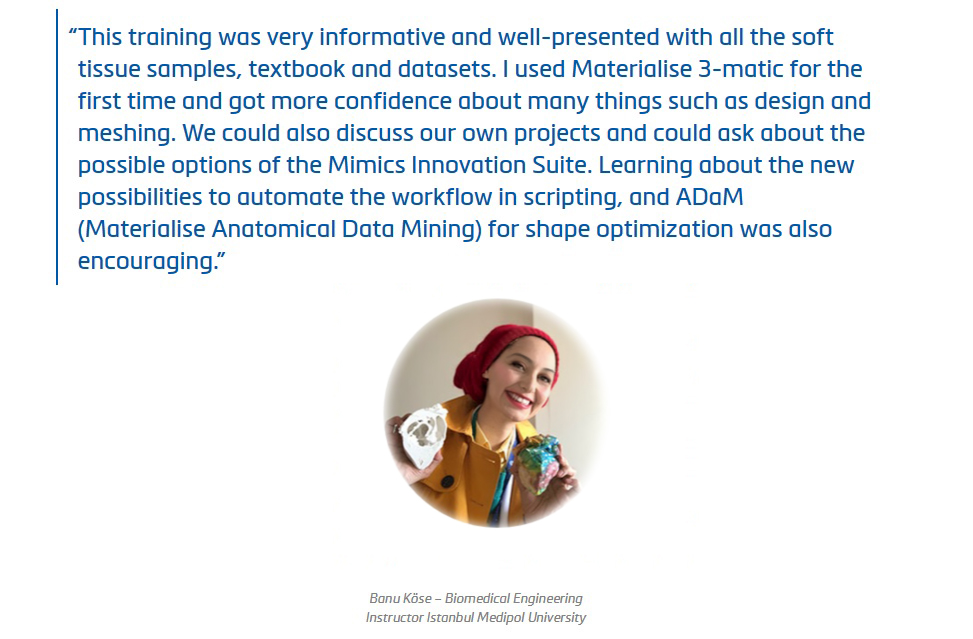
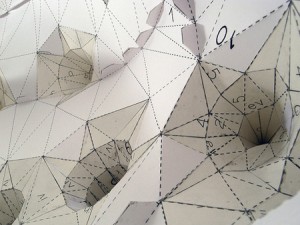
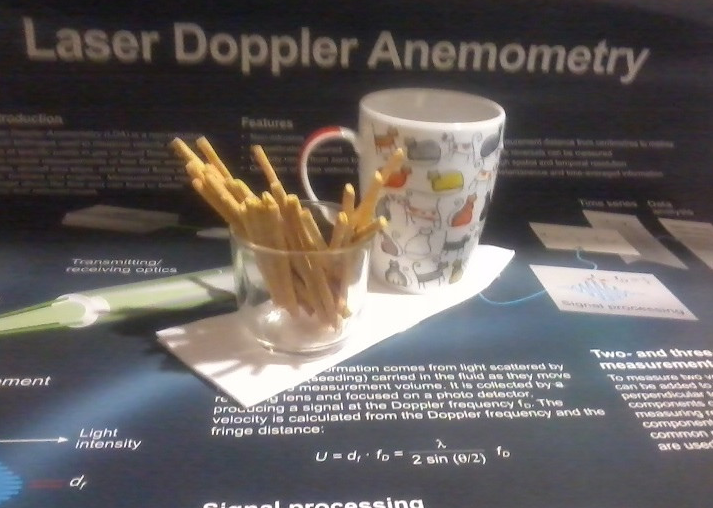
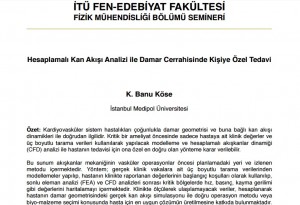
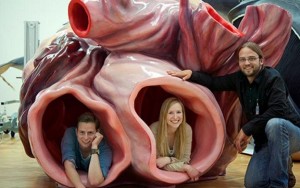
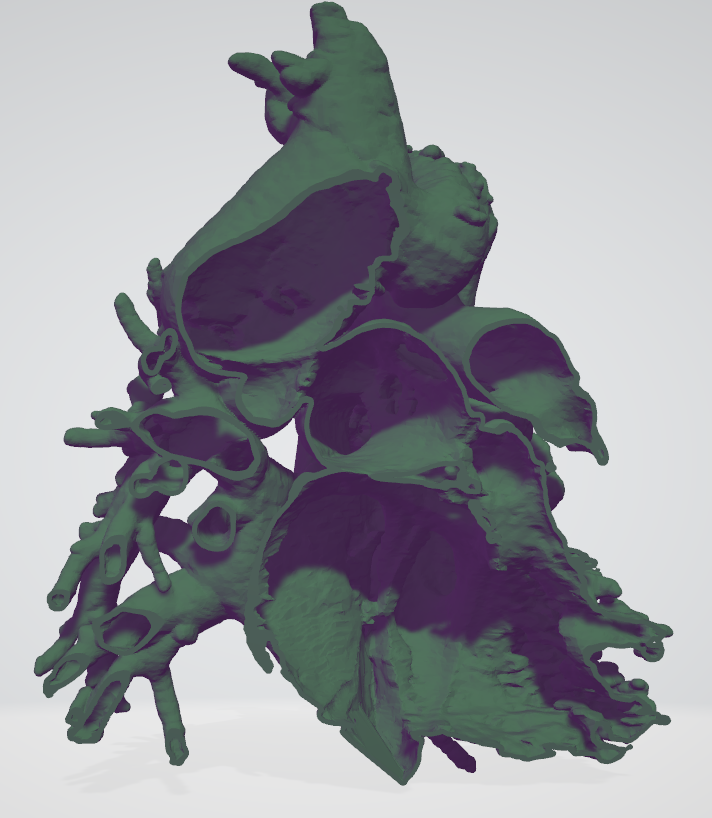
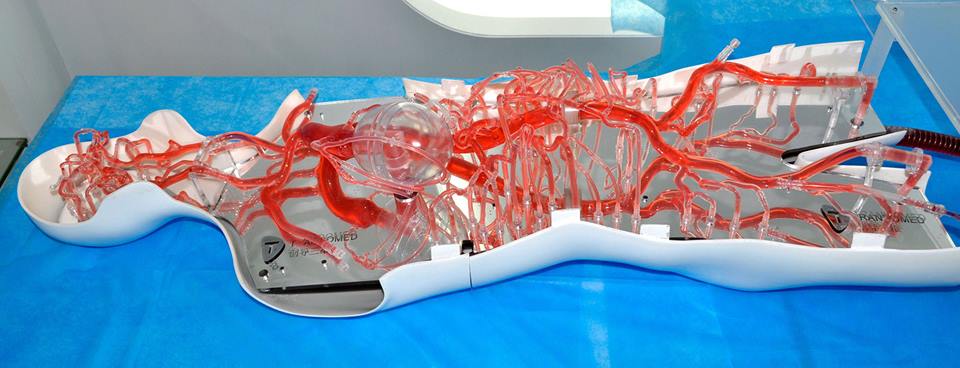
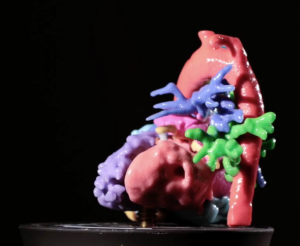
![]() 3D Printing, 3D Slicer, ANSYS, Art, Artificial Organs, Banu Köse, Banu Pluie, BioFluidLab, Bioengineering, Biomaterials, Biomechanics, Biomed, Biomedical Science, Biophysics, Bioprinting, Biosecience, Cardiology, Cardiovascular Implants, Cerrahi, Circulatory Support Systems, ClinicianEngineerHub, Complex Systems, Congenital, Ece Salihoglu, Engineering, Finite Element Model, Fontan, Gradute, Heart, Heart Valves, Hemodynamics, Hepatic, IMAEH, Image Processing, K. Banu Köse, Kardiyovasküler, Kardiyovasküler Mekanik, Kevser Banu Köse, Laser Doppler, Liquid State, Materialise Medical, Medipol, Medtronic, Pediatric, Perfusion, Perfüzyon, PhD, Physics, Pulmonary, Radiology, Slicer, Structural Analysis, Surgery, SurgicalPlanning, Sıvı Hal Fiziği, TGA, The Journal of Cardiovascular Surgery, VSD, VirtalSurgery, Virtual Physiological Human, Windkessel, WomenEngineers, womenin3d
3D Printing, 3D Slicer, ANSYS, Art, Artificial Organs, Banu Köse, Banu Pluie, BioFluidLab, Bioengineering, Biomaterials, Biomechanics, Biomed, Biomedical Science, Biophysics, Bioprinting, Biosecience, Cardiology, Cardiovascular Implants, Cerrahi, Circulatory Support Systems, ClinicianEngineerHub, Complex Systems, Congenital, Ece Salihoglu, Engineering, Finite Element Model, Fontan, Gradute, Heart, Heart Valves, Hemodynamics, Hepatic, IMAEH, Image Processing, K. Banu Köse, Kardiyovasküler, Kardiyovasküler Mekanik, Kevser Banu Köse, Laser Doppler, Liquid State, Materialise Medical, Medipol, Medtronic, Pediatric, Perfusion, Perfüzyon, PhD, Physics, Pulmonary, Radiology, Slicer, Structural Analysis, Surgery, SurgicalPlanning, Sıvı Hal Fiziği, TGA, The Journal of Cardiovascular Surgery, VSD, VirtalSurgery, Virtual Physiological Human, Windkessel, WomenEngineers, womenin3d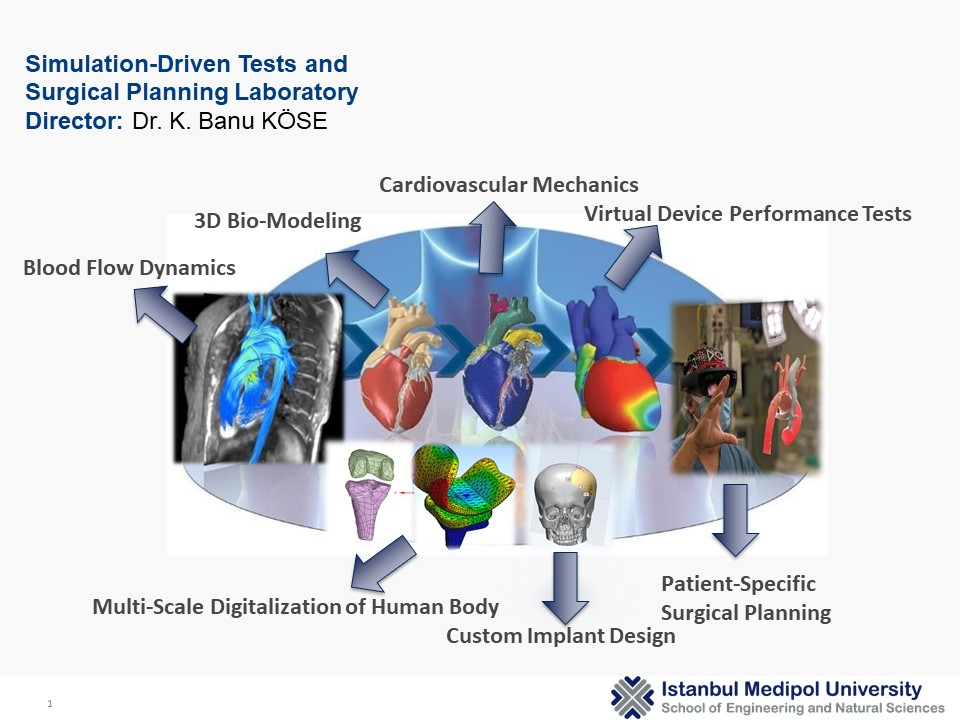










































 http://gsse.ku.edu.tr
http://gsse.ku.edu.tr